Community Concussion Discussion
Posted September 2, 2015 at 11:02 am by Tim Dustrude

Article Submission from San Juan Island School District
September 2, 2015
The San Juan Island School District and the sports community are in the process of improving procedures for concussions.
The tragic effects among professional athletes have focused national media on concussions. Locally, the concern is the treatment of our children and addressing misconceptions about what concussions are and what the implications of these injuries are.
Part 1 of this article will focus on what concussions are and the effects they can have, what our local data is. Part 2 will update everyone on how we are changing to incorporate evolving best practice.
Part 1
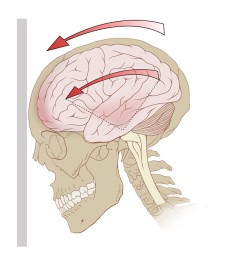
The brain is a gelatinous supercomputer in a bone box. When a blow occurs, it bumps about inside the box. The blows come from any number of sources: the ground, a car windshield, another head, or a helmet. Even protective head gear cannot stop the rattling and bruising of the brain. In the young adult, this fragile instrument is growing and changing. During a concussion tenuous connections get stretched, micro-bruised, and sometimes broken. Nothing may appear to be wrong. Helmets do dampen severe injuries so tests such as CT scans and MRIs can give a false “normal” result.
Damage ranges from briefly “seeing stars”, to dizziness, confusion, memory loss, or unconsciousness. Too often in the past, only the most obvious symptoms were taken seriously, and the child resumed their individual activity or was put back in the game.
Most kids who resume their activities are fine after a concussion. But many have persistent effects. They may have trouble paying attention, become distractible, and have fatigue, dizziness, headaches, blurred vision, nausea, and surges of emotion. Bright lights, loud noises, and screen exposure may worsen these symptoms. Such problems may continue for weeks or months resulting in major impacts in school and daily life.
Another blow to the head soon after the first can be disastrously life changing. This happened to Tahoma high school student Zachary Lystedt who became permanently disabled following a second concussion. His parents championed legislation culminating in Washington becoming the first in the nation to legislate what is needed for a child to resume school sports: now, only a medical professional can permit a child to return to play. Because less than half of youth aged concussions happen in supervised sports, a tracking and management system to capture all concussions is the logical next step.
From November 2011 to August 2015, San Juan Health Care treated 30 childhood concussions, plus 7 repeats. Of the 37 events, 17 occurred during school sports but 20 happened elsewhere including falls from horses, automobile accidents, and trampoline injuries. Half had rapid resolution while the other half had symptoms lasting long enough to require temporary modification of their school program. A quarter had findings lasting months to years. This is an under count as there is no community-wide database of concussions. Neither are there uniform methods to determine exclusion or approval for full participation. In Part 2 we will present our plan to improve our response to concussions and their management.
Part Two
It is clear we needed to have a uniform education and evaluation program to better address youth concussions. A public school based group was established last spring and assigned the following tasks:
- Teach the community about concussions, the process of removal from play, and medical management, emphasizing coach and parent education and responsibility. Reinforce coach training programs already in place. Focus on helping parents understand the need to make coaches, medical providers, and teachers aware of all head injuries not just those sustained in organized sports.
- Perform preseason screening to establish cognitive baselines that allow rapid accurate assessment of mental status following a suspected concussion. Such tools do not diagnose but simply determine the need to exclude an injured participant from play pending appropriate medical assessment. The use of such tools allows coaches to depersonalize exclusion from play.
- Formalize policies and procedures for return to play and for structured modification of the academic program of an injured player.
- Work with others in the community to establish an island-wide data base that allows for tracking while ensuring appropriate privacy protection.
To meet these four goals, talks to various sports groups and schools have begun and public presentations of nationally recognized films will be scheduled in the near future. We are also implementing a proven screening protocol.
The King-Devick visual tracking system is being piloted at Friday Harbor High School. This instrument is a validated, inexpensive, and easily administered tool that uses eye movements and a number display. It is quick and easily administered and a proven assessment of clear mental function. If a concussion is suspected, the test is quickly re-performed and compared to the pre-season baseline. If there is a significant deviation, they will be immediately be removed. Only when a medical provider clears the athlete and notifies the Athletic Director, can practice and play can be resumed. If there is any question regarding the player’s mental status, they will be removed regardless of the test result.
There are now established assessments for medical providers to more objectively evaluate concussions and their course. These have most often been used in academic centers but are now moving towards broad application. These include the Sport Concussion Assessment Tool Version 3 (SCAT3) and the Balance Error Scoring System (BESS). Like the King-Devick, these are standardized and simply administered tests that guide the provider, the coaches, and the teaching staff in assessing the student’s recovery.
We will individualize both a modified academic program and a structured return to play. If a child sustains a severe injury, has had multiple events, or has an unusually long recovery period a referral to the Concussion Clinic at Children’s Hospital will occur.
Once these procedures are debugged at the High School, the next goal will be to disseminate them Island wide to all our community sports and youth activity organizations. The more information we all have, and by consistently applying best practices, the better outcomes will be for our children with concussions.
San Juan Island School District Concussion Committee:
Mark Fishaut MD FAAP, Pediatrician
Jack McKenna, Chairman School Board
Rod Turnbull, Athletic Director
Beck M. Bell, Director of Special Education
Danna Diaz, School Superintendent
You can support the San Juan Update by doing business with our loyal advertisers, and by making a one-time contribution or a recurring donation.
Categories: Around Here









No comments yet. Be the first!
By submitting a comment you grant the San Juan Update a perpetual license to reproduce your words and name/web site in attribution. Inappropriate, irrelevant and contentious comments may not be published at an admin's discretion. Your email is used for verification purposes only, it will never be shared.